Introduction
When it comes to overcoming addiction, therapy plays a crucial role in providing individuals with the tools and strategies necessary to achieve long-term recovery. Two of the most widely used and effective therapeutic approaches are Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT). While both therapies aim to help individuals change harmful behaviors and thought patterns, they differ in their core principles, techniques, and areas of focus.
In this article, we’ll explore the key differences between CBT and DBT, their effectiveness in addiction treatment, and how to determine which approach may be best for you or your loved one.
What is Cognitive Behavioral Therapy (CBT)?
CBT is a structured, goal-oriented form of psychotherapy that focuses on identifying and changing negative thought patterns and behaviors. Developed in the 1960s, CBT has become one of the most effective treatments for mental health conditions such as depression, anxiety, and addiction.
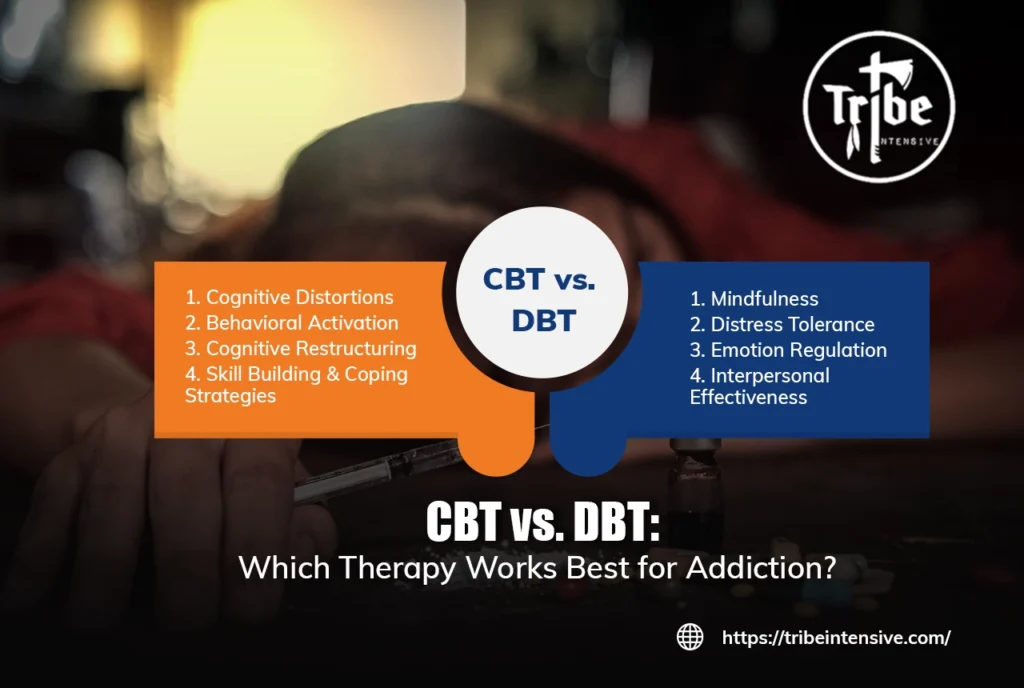
Key Components of CBT:
- Cognitive Distortions: Identifying and correcting irrational or harmful thought patterns that contribute to addiction.
- Behavioral Activation: Encouraging positive behaviors to replace substance use.
- Cognitive Restructuring: Changing negative thought patterns to promote healthier decision-making.
- Skill Building & Coping Strategies: Developing tools to manage cravings, stress, and relapse triggers.
CBT helps individuals recognize how their thoughts influence their emotions and behaviors. By addressing these thought patterns, people can break free from destructive cycles and make healthier choices.
What is Dialectical Behavior Therapy (DBT)?
DBT is a specialized form of cognitive therapy initially developed to treat borderline personality disorder (BPD). However, it has since proven highly effective for addiction treatment as well. DBT focuses on emotional regulation, distress tolerance, and interpersonal effectiveness, making it a valuable approach for those struggling with intense emotions and impulsive behaviors.
Key Components of DBT:
- Mindfulness: Encouraging self-awareness and present-moment focus to reduce impulsive decision-making.
- Distress Tolerance: Teaching skills to cope with uncomfortable emotions without turning to substances.
- Emotion Regulation: Helping individuals understand, manage, and respond to emotions in a healthy way.
- Interpersonal Effectiveness: Improving communication and relationship-building skills to foster healthier social interactions.
Unlike CBT, which primarily focuses on thought patterns, DBT emphasizes acceptance, emotional balance, and developing strategies to cope with distressing situations.
CBT vs. DBT: Key Differences in Addiction Treatment
While both CBT and DBT have been proven effective in addiction treatment, their approaches differ in several key areas:
| Feature | Cognitive Behavioral Therapy (CBT) | Dialectical Behavior Therapy (DBT) |
|---|---|---|
| Focus | Changing negative thought patterns | Emotional regulation and distress tolerance |
| Core Strategy | Identify and replace harmful thoughts | Accept emotions while managing behaviors |
| Effectiveness for Addiction | Strong for treating substance abuse and relapse prevention | Best for individuals with co-occurring emotional dysregulation |
| Skills Taught | Cognitive restructuring, coping mechanisms | Mindfulness, emotion regulation, distress tolerance |
| Who Benefits Most? | Individuals with harmful thought patterns | Individuals with intense emotions or impulsive behaviors |
While CBT is highly effective for individuals who struggle with negative thought patterns and self-defeating beliefs, DBT is particularly useful for those who experience intense emotional dysregulation and impulsivity, which can often lead to substance abuse.
How Effective are CBT and DBT for Addiction Recovery?
Research shows that both CBT and DBT can significantly improve addiction treatment outcomes. Here’s how they contribute to recovery:
Effectiveness of CBT:
- Studies indicate that CBT is one of the most effective forms of therapy for substance use disorders (SUDs).
- CBT helps individuals develop coping skills that reduce cravings and prevent relapse.
- It is particularly beneficial for those with co-occurring anxiety or depression.
Effectiveness of DBT:
- DBT has been shown to be highly effective for individuals struggling with both addiction and emotional dysregulation.
- Research suggests that DBT reduces impulsivity and helps individuals manage intense emotions that can trigger substance use.
- It is especially useful for those with co-occurring disorders such as borderline personality disorder (BPD) or PTSD.
Choosing the Right Therapy: CBT or DBT?
Determining whether CBT or DBT is the right therapy for addiction recovery depends on the individual’s specific needs. Here are some factors to consider:
- Choose CBT if:
- You struggle with negative thought patterns that drive addiction.
- You need structured, goal-oriented therapy to manage triggers.
- You want to develop coping skills to prevent relapse.
- Choose DBT if:
- You experience extreme emotional highs and lows that lead to substance use.
- You need skills to regulate emotions and tolerate distress without using substances.
- You want to improve interpersonal relationships and communication skills.
In many cases, therapists use a combination of both CBT and DBT to tailor treatment plans to individual needs
CBT and DBT are both highly effective therapeutic approaches for addiction recovery, each offering unique benefits. While CBT helps individuals change negative thought patterns and develop coping skills, DBT focuses on emotional regulation and distress tolerance.
Choosing the right therapy depends on the individual’s personal struggles, emotional needs, and addiction triggers. Seeking professional guidance from a therapist or addiction specialist can help determine the best course of treatment for long-term recovery.
If you or a loved one is struggling with addiction, consider exploring CBT, DBT, or a combination of both to find a tailored approach that supports your journey to sobriety.
For more information and professional addiction treatment resources, visit Tribe Intensive.